Management of Chronic Subdural Hematomas with Subdural Evacuation Port System: A Single Center Retrospective Review
Keywords:
chronic subdural hematoma, burr hole, subdural hematoma, Brain tumorsAbstract
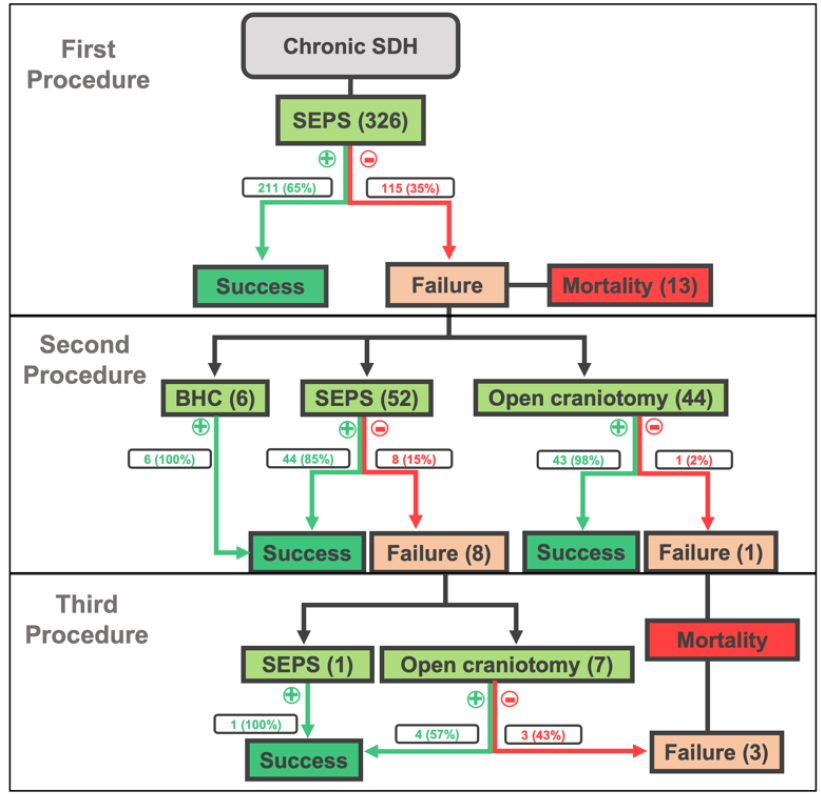
Objective: Chronic subdural hematoma (cSDH) is prevalent globally and its management is evolving to minimize morbidity while optimizing theater utilization. We present our institution’s experience with subdural evacuation port system (SEPS) as a first-line treatment approach to cSDHs. Methods: A retrospective review was performed of patients undergoing bedside SEPS placement in a single institution. Pre- and post-procedural radiographic and clinical data were collected and analyzed to identify predictive variables of procedural success for the SEPS approach. For procedure failures, subsequent procedures were analyzed for rates of success. Results: 268 patients were identified for a total of 326 initial procedures. Pre-procedural variables associated with improved odds of a good outcome were: unilateral cSDH, prior use of anticoagulation, GCS > 13 at presentation, larger cSDH, and greater degree of midline shift (MLS). 65% success rate was observed for initial SEPS placement and an overall success of 78% after repeat SEPS. Patients with subsequent failures underwent craniotomy. Conclusions: Bedside SEPS placement is a low-risk option for first-line treatment of cSDH and may spare patients from the risks of general anesthesia while reducing burden on surgical theaters in resource-limited settings. Performing a repeat SEPS procedure is a reasonable surgical option if the first procedure fails to completely evacuate the cSDH.
References
Hoffman H, Ziechmann R, Beutler T, Verhave B, Chin LS. First-line management of chronic subdural hematoma with the subdural evacuating port system: Institutional experience and predictors of outcomes. J Clin Neurosci. 2018;50:221-5.
Karibe H, Kameyama M, Kawase M, Hirano T, Kawaguchi T, Tominaga T. [Epidemiology of chronic subdural hematomas]. No Shinkei Geka. 2011;39(12):1149-53.
Lee JY, Ebel H, Ernestus RI, Klug N. Various surgical treatments of chronic subdural hematoma and outcome in 172 patients: is membranectomy necessary? Surg Neurol. 2004;61(6):523-7; discussion 7-8.
Ernestus RI, Beldzinski P, Lanfermann H, Klug N. Chronic subdural hematoma: surgical treatment and outcome in 104 patients. Surg Neurol. 1997;48(3):220-5.
Firsching R, Frowein RA, Thun F. Encapsulated subdural hematoma. Neurosurg Rev. 1989;12 Suppl 1:207-14.
Svien HJ, Gelety JE. On the Surgical Management of Encapsulated Subdural Hematoma. A Comparison of the Results of Membranectomy and Simple Evacuation. J Neurosurg. 1964;21:172-7.
Geller AI, Shehab N, Lovegrove MC, Rose KO, Weidle NJ, Goring SK, et al. Emergency Visits for Oral Anticoagulant Bleeding. J Gen Intern Med. 2020;35(1):371-3.
Weigel R, Schmiedek P, Krauss JK. Outcome of contemporary surgery for chronic subdural haematoma: evidence based review. J Neurol Neurosurg Psychiatry. 2003;74(7):937-43.
Flint AC, Chan SL, Rao VA, Efron AD, Kalani MA, Sheridan WF. Treatment of chronic subdural hematomas with subdural evacuating port system placement in the intensive care unit: evolution of practice and comparison with bur hole evacuation in the operating room. J Neurosurg. 2017;127(6):1443-8.
Link TW, Rapoport BI, Paine SM, Kamel H, Knopman J. Middle meningeal artery embolization for chronic subdural hematoma: Endovascular technique and radiographic findings. Interv Neuroradiol. 2018;24(4):455-62.
Ng S, Derraz I, Boetto J, Dargazanli C, Poulen G, Gascou G, et al. Middle meningeal artery embolization as an adjuvant treatment to surgery for symptomatic chronic subdural hematoma: a pilot study assessing hematoma volume resorption. Journal of NeuroInterventional Surgery. 2019:neurintsurg-2019-015421.
Fiorella D, Arthur AS. Middle meningeal artery embolization for the management of chronic subdural hematoma. J NeuroInterv Surg. 2019;11(9):912-5.
Iorio-Morin C, Touchette C, Levesque M, Effendi K, Fortin D, Mathieu D. Chronic Subdural Hematoma: Toward a New Management Paradigm for an Increasingly Complex Population. J Neurotrauma. 2018;35(16):1882-5.
Rauhala M, Luoto TM, Huhtala H, Iverson GL, Niskakangas T, Ohman J, et al. The incidence of chronic subdural hematomas from 1990 to 2015 in a defined Finnish population. J Neurosurg. 2019:1-11.
Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 2001;95(2):256-62.
Stanisic M, Pripp AH. A Reliable Grading System for Prediction of Chronic Subdural Hematoma Recurrence Requiring Reoperation After Initial Burr-Hole Surgery. Neurosurgery. 2017;81(5):752-60.
Automated Preoperative and Postoperative Volume Estimates Risk of Retreatment in Chronic Subdural Hematoma: A Retrospective, Multicenter Study. Neurosurgery. 2023.
Lukasiewicz AM, Grant RA, Basques BA, Webb ML, Samuel AM, Grauer JN. Patient factors associated with 30-day morbidity, mortality, and length of stay after surgery for subdural hematoma: a study of the American College of Surgeons National Surgical Quality Improvement Program. J Neurosurg. 2016;124(3):760-6.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 East African Journal of Neurological Sciences

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.